A mechanism, biomarker, and potential therapeutic target
Alzheimer’s disease (AD) is a neurodegenerative disease that currently accounts for around two-thirds of all dementia cases, but AD incidence is rapidly increasing, predicted to grow from approximately 47 million global sufferers in 2015 to 75 million by 2030(1).
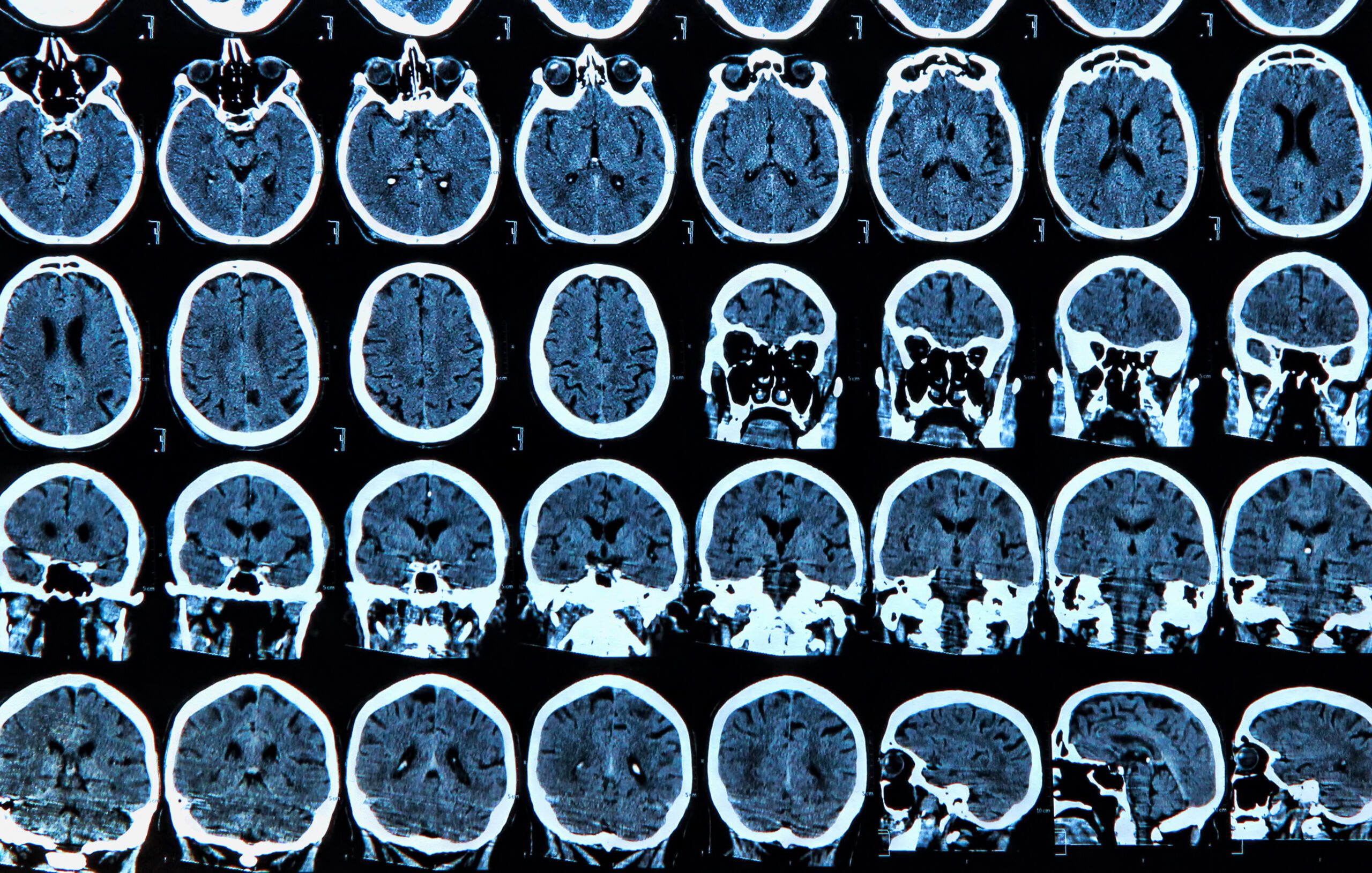
It is characterised by a number of pathological features: presence of Amyloid beta (Aβ) plaques and neurofibrillary tangles formed by tau protein hyperphosphorylation that spread throughout the brain, as well as general neuronal cell loss and reduced synaptic capacity. These features are reported to start proliferating long before symptoms are visible, some suggesting at least 15 years(2).
It is well known that AD has a range of genetic components, being described as a polygenic disease where many common genetic variants all have small contributions to the overall disease risk.
Recently, DNA methylation has also been heavily implicated in AD and other neurodegenerative diseases, and changes in DNA methylation patterns in the brain have been identified as contributing to, or a marker of, AD progression. Here, we review a selection of publications investigating the role of genetics and DNA methylation in AD.
DNA methylation can explain over a third of gene expression changes in Alzheimer’s
Genome-wide studies of DNA methylation attempt to associate changes in methylation levels/patterns with incidence of disease. Such studies are regularly being performed for AD and other neurodegenerative diseases in order to discover potential genetic and epigenetic pathways that could contribute to disease risk or even mechanism.
Wang et al(3) identified a range of differentially methylated regions (DMRs) associated with AD, and further integrated these with gene expression (from RNA transcriptomics) and proteomic data from the same brain regions in the same human subjects to investigate regulatory consequences of DNA methylation in AD.
They showed that DNA methylation could explain on average 34% (with a range of 13-61% depending on the genetic region in question) of gene expression alterations in AD, and 39% of protein expression variance.
They specifically investigated a high-ranked key driver gene (that had high contribution to AD risk) HTR2A, which is related to biological pathway signalling, showing that this particular gene is down-regulated in AD, and had low protein expression, consistent with a nearby DMR with high levels of methylation.
They demonstrated the pattern of associated DNA methylation with gene and protein expression in high-risk AD genes multiple times, suggesting that these genes could represent potential therapeutic targets.
Their work shows that DNA methylation has a key role in the regulation of gene networks associated with AD, and investigating both key genetic changes and DNA methylation changes is important for investigating this disease.
5hmC appears 10-fold higher in the brain and has a crucial role in Alzheimer’s development
DNA methylation is split into 4 different cytosine modifications, the most common being 5-methylcytosine (5mC) which has a significantly higher prevalence in the human genome than any others.
The second most common methylation mark is 5-hydroxymethylcytosine (5hmC), which is present at far fewer positions in the human genome but is enriched 10-fold higher in brain than peripheral tissues, suggesting a unique function within neuronal systems.
Zhang et al(4) used mouse brain models to investigate how 5hmC may play a unique role in AD, building on previous demonstrations that 5hmC levels can change significantly with etiology of the disease.
They show that a genome-wide reduction in 5hmC levels is seen in neurons, but not astrocyte cells, in the mouse AD model.
They link this 5hmC reduction to a decrease in TET activity, the enzyme that catalyses the conversion of 5mC to 5hmC. Decreased TET activity has also been shown in the brains of humans who died with AD, and they suggest that this could be the cause for the reduction in 5hmC.
They further investigate the relationship between 5hmC, TET and AD by overexpressing human TET catalytic domains in the mouse AD models, which results in a significant attenuation of the neurodegenerative process with reduced Aβ accumulation and Tau protein hyperphosphorylation. These results reflect the crucial role of 5hmC and its deregulation in the events leading up to AD neurodegeneration.
Non-neuronal cells are also important…
Non-neuronal cells have also been shown to play key roles in neurodegeneration and AD. Fodder et al(5) review the role of oligodendrocytes in AD, and how DNA methylation can contribute to their dysfunction.
The primary function of oligodendrocytes is to produce myelin, the membrane that wraps around neuronal axons and enables electrical transmission between neurons.
Changes in neuron myelination are implicated in a range of neurodegenerative diseases including AD, with the natural age-related decline in myelination occurring at the same time as typical onset of these conditions (approximately 60 years old).
Myelin loss does not occur uniformly across the brain: areas where AD symptoms are more likely to present early are also areas where myelin reduction occurs sooner, and loss of myelin integrity can act as a predictor for AD.
There are indications that changes in the number and morphology of oligodendrocytes occurs in AD, and specific oligodendrocyte genes have been implicated in neurodegeneration.
BIN1 is the second strongest genetic risk factor for late onset AD, and is largely expressed in oligodendrocytes. Oligodendrocyte-related genes are often differentially methylated in AD, and BIN1 levels have been linked with Aβ load.
Moreover, Fodder et al describe how DNA methylation is dynamic in the process of precursor cells differentiating into oligodendrocytes.
Removal of DNMT, the enzyme responsible for methylation of cytosines, results in an overall reduction of myelination due to lack of precursor cells proliferating, resulting in less mature oligodendrocytes available for myelination.
In the brains of AD sufferers, an increased number of these precursor cells is observed, which could be reflective of a lack of oligodendrocyte differentiation resulting in overall lower myelination levels.
The potential for DNA methylation in Alzheimer’s detection
DNA methylation is also being explored as a biomarker for AD. Multiple studies have identified altered DNA methylation profiles associated with the disease, including the HOXB6 gene that shows hypermethylation in AD(6), 5hmC signatures illustrative of AD(7), and other blood-born methylation biomarkers(8, 9). These represent a range of targets that could be used to detect whether somebody is suffering from AD.
The ultimate goal is to identify a biomarker, whether a genetic variant, a DNA methylation profile, or likely a combination of the two, that can be used to predict AD onset early, before other symptoms appear. This offers the highest likelihood of treating the disease.
These publications highlight the importance of measuring both genetic and methylation changes when studying or testing for AD.
Disease-associated epigenetic changes are potentially reversible and therefore offer targets for therapeutic intervention. But in order to actionably target these areas, the full extent of their effect across all biological functions on which they act must be understood, and this cannot be achieved without exploring both genetics and epigenetics.
Appendix
- Prince, Martin, et al. World Alzheimer report 2015. The global impact of dementia: an analysis of prevalence, incidence, cost and trends. Diss. Alzheimer’s disease international, 2015.
- Smith, A R et al. “Invited Review – A 5-year update on epigenome-wide association studies of DNA modifications in Alzheimer’s disease: progress, practicalities and promise.” Neuropathology and applied neurobiology vol. 46,7 (2020): 641-653. doi:10.1111/nan.12650
- Wang, Erming et al. “Genome-wide methylomic regulation of multiscale gene networks in Alzheimer’s disease.” Alzheimer’s & dementia : the journal of the Alzheimer’s Association vol. 19,8 (2023): 3472-3495. doi:10.1002/alz.12969
- Zhang, Ying et al. “Selective loss of 5hmC promotes neurodegeneration in the mouse model of Alzheimer’s disease.” FASEB journal : official publication of the Federation of American Societies for Experimental Biology vol. 34,12 (2020): 16364-16382. doi:10.1096/fj.202001271R
- Fodder, Katherine et al. “The contribution of DNA methylation to the (dys)function of oligodendroglia in neurodegeneration.” Acta neuropathologica communications vol. 11,1 106. 29 Jun. 2023, doi:10.1186/s40478-023-01607-9
- Roubroeks, Janou A Y et al. “An epigenome-wide association study of Alzheimer’s disease blood highlights robust DNA hypermethylation in the HOXB6 gene.” Neurobiology of aging vol. 95 (2020): 26-45. doi:10.1016/j.neurobiolaging.2020.06.023
- Chen, Lei et al. “5-Hydroxymethylcytosine Signatures in Circulating Cell-Free DNA as Diagnostic Biomarkers for Late-Onset Alzheimer’s Disease.” Journal of Alzheimer’s disease : JAD vol. 85,2 (2022): 573-585. doi:10.3233/JAD-215217
- Wu, Shaochang et al. “Altered DNA methylome profiles of blood leukocytes in Chinese patients with mild cognitive impairment and Alzheimer’s disease.” Frontiers in genetics vol. 14 1175864. 14 Jun. 2023, doi:10.3389/fgene.2023.1175864
- Schäfer Hackenhaar, Fernanda et al. “Sixteen-Year Longitudinal Evaluation of Blood-Based DNA Methylation Biomarkers for Early Prediction of Alzheimer’s Disease.” Journal of Alzheimer’s disease : JAD vol. 94,4 (2023): 1443-1464. doi:10.3233/JAD-230039